
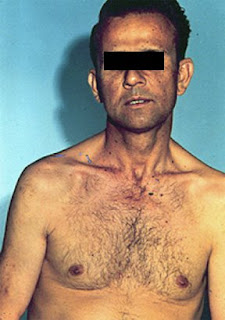
look at the eyes of this patient.
what is defferential diagnosis?
Dear friends and colleagues, Passing the MRCP UK is an important step in the medical career. PACES is the practical clinical exam and require a wide breadth of knowledge. This blog is a space to share materials, information and knowledge and I hope you find it useful. Am open for any ideas or suggestion and would value your contributions and comments. please visit my related pages on facebook and youtube. Best wishes, Dr Elmuhtady Said

In one study, physicians did not allow patients to complete their opening statements 69% of the time. The mean time until the first interruption was 18 seconds. Once interrupted, fewer than 2% of patients went on to complete their statements.
"Data are thus very much physician-determined, skewed toward problems that are biomedical in nature... It has been proposed that current interviewing practices are at odds with scientific requirements: They produce biased, incomplete data about the patient."
Goal: To establish a favorable context for the interview
Welcome the patient
Know and use the patient's name
Introduce and identify yourself
Ensure comfort and privacy
Goal: To establish the agenda for the interview
Obtain list of all issues - avoid detail
Chief Complaint
Other complaints or symptoms
Specific requests (i.e. medication refills)
Patient's expectations for this visit
Ask the patient "Why now?"
Goal: To establish a good flow of information
Open-ended questions initially
Encourage with silence, nonverbal cues, and verbal cues
Focus by paraphrasing and summarizing
Goal: To smoothly shift into physician-centered interviewing
Summarize interview up to that point
Verbalize your intention to make the transition
This should be clear from the transition summary.
Move from general to specific
Flow from open-ended to closed-ended questions
Allergies/Adverse Reactions
Medications/Immunizations
Major Medical or Psychiatric Problems/Major Surgeries
Last Menstrual Period/Pregnancies/Contraception (if female)
Smoking/Alcohol/Caffeine/Other Drugs
Family/Social History
Occupational History
Sexual History





























%5B1%5D.JPG)


